Beat Posterior Tibial Tendonitis - How Orthotics Can Help
2022 Sep 12th
Posterior Tibial Tendonitis, also called Posterior Tibial Tendon Dysfunction (PTTD) or Posterior Tibial Tendon Insufficiency, is the tearing of the Tibialis Posterior Tendon, or the sudden or gradual loss in strength of the Tibialis Posterior Tendon. Posterior Tibial Tendonitis is a painful condition that aggravates the foot and ankle. Posterior Tibial Tendonitis can impact your ability to walk, run, and perform lower-body movements.
The Posterior Tibial Tendon resides under the bone in the upper ankle. It connects your calf muscle to bones on the inside of your foot. The tendon acts as the main stabilizing element in the lower leg and supports the arch on the inside of your foot, preventing it from slipping. If injured or overused, the tendon gets irritated and/or begins to degrade. If your posterior tibial tendon is injured or breaks down, it can fail to support your arch.
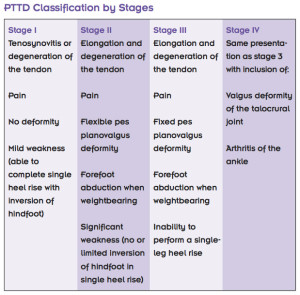
Four Stages of Posterior Tibial Tendon Dysfunction:
- Stage I: The Tendon is injured, but otherwise intact.
- Stage II: The Tendon is torn (ruptured) or not working properly. The foot is deformed.
- Stage III: The foot is significantly deformed. There are degenerative changes to the connective tissue (cartilage) in the back of the foot.
- Stage IV: There are degenerative changes to the ankle joint.
With proper diagnosis and treatment, the outlook for people with Posterior Tibial Tendon Dysfunction is good. Orthotics can make a significant difference in preventing, healing, and managing Posterior Tibial Tendon Dysfunction.
Symptoms of Posterior Tibial Tendonitis
Posterior Tibial Tendonitis symptoms include visible inflammation (swelling) along the tendon, stiffness in the ankle, sharp pains along the inner part of the foot or ankle, a popping sensation, and soreness to the touch.
Orthotics are one of the most common and effective treatments of Posterior Tibial Tendon Dysfunction (Posterior Tibial Tendonitis)
Our staff Orthotic Technicians continually work to improve access to affordable Orthotics to help more people suffering with the affects of Posterior Tibial Tendonitis. It is a simple and cost effective treatment to address a painful condition.
Symptoms of Posterior Tibial Tendonitis
The most common Posterior Tibial Tendonitis symptoms are pain and/or swelling of the foot or ankle. Ankle rolling and popping are common to this condition.
- Pain Standing on Your Toes
- Ankle Rolls Inward or Pops
- Difficulty Walking on Uneven Terrain / Surfaces
- Difficulty Walking Stairs
Indicators of Posterior Tibial Tendonitis
Uneven wear on shoe soles can be an indication of this condition, as can difficulty walking on uneven terrain and stairs.
What is the Posterior Tibial Tendon?
The posterior tibial tendon is a strong cord of tissue about as think as a pencil. The Tendon inserts into your foot along your instep, runs up beside the medial malleolus (the large bump on the inside of your ankle), and attaches to the tibialis posterior muscle, buried deep inside your calves. The posterior Tibialis Tendon is one of the most important tendons in your leg.
What Causes Posterior Tibial Tendonitis?
High impact physical activity, trauma, and repetitive use can injure the Posterior Tibial Tendon. The Tendon degrades with age. Obesity causes the tendon to break down faster. Previous foot and ankle injuries can speed degradation of the Posterior Tibial Tendon. It is widely believed that repetitive stress and small tendon injuries caused by a sudden increase in activity are the most common cause of Posterior Tibial Tendonitis
The overall incidence of this disease, it is believed that the prevalence is anywhere from 3.3 to 10%, depending on the sex and age of the patient. Diabetes, hypertension, obesity, previous surgery, foot/ankle trauma and steroid use, are found in up to 60% of patients. Posterior Tibial Tendonitis is associated with adult-acquired flatfoot deficiency which can cause it to be misdiagnosed, meaning the actual prevalence may be much higher than shown in the literature.[2]
Key Contributing Factors to Posterior Tibial Tendonitis:
- Older Age
- Being Overweight
- Diabetes
- Inflammatory Conditions (Rheumatoid Arthritis, Psoriatic Arthritis, etc.)
- Weakness and/or Tightness of Feet and/or Leg Muscles
- Wearing Unsupportive Footwear, such as Sandals
- Long Periods of Standing, Walking, Running,
, and Sudden Increase in these Activities - Poor Exercising and/or Training Technique
- Poor / Short Exercise Recovery Times
- Prolonged use of oral corticosteroids and a certain family of antibiotics (fluoroquinolones)
- Previous Foot and Ankle Injury
- High Impact Sports
Repetitive Stress causes Posterior Tibial Tendonitis.
Repetitive stress injuries slow the tendon's natural healing response, causing injury to occur fasted than the body can heal them. This compounded injury leads to a weakening of the Tendon. Weakened Tendons are more vulnerable to reinjury.
Is Posterior Tibial Tendonitis Common? Absolutely.
Posterior Tibial Tendonitis affects 3.3-10% of populations, most commonly occurring among women aged 40-50. The condition typically affects only one foot.
Who does Posterior Tibial Tendonitis affect?
Posterior tendon damage is most common among obese women of middle age (10% incidence). It commonly affects individuals who are or have:
- Obesity.
- High Blood Pressure (hypertension)
- Diabetes
- Foot or Ankle Injuries
- Joint Disorders
- Prior Surgery
- Steroid Use
- High Impact Sport Athletes / Injury Sufferers (football, basketball, soccer, track, distance running, in particular).
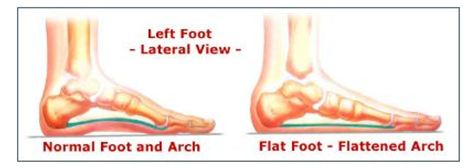
Posterior Tibial Tendonitis is the most common cause of adult-acquired flatfoot
Flatfoot is a very common condition affecting the feet and ankles of women and men. Flatfoot occurs when the arch of the foot falls or collapses. Flatfoot is painful, even debilitating. Adult flatfoot is effectively treated with orthotics and other non-surgical treatments.
Treatment - Posterior Tibial Tendonitis
The most common treatments of Posterior Tibial Tendonitis are non-surgical. They are: Reducing stress on the Tendon, using a corrective orthotic, stretching of the lower leg, and strengthening the surrounding areas.
- Orthotics: Over-the-counter shoe inserts provide support for your tendon and arch. Healthcare providers may prescribe custom orthotic insoles, a walking boot or cast, or custom orthotic brace(s) specifically molded to your foot.
- Rest: Limit high impact activity and actions that aggravate your Tendon. Switch to low-impact exercises like bicycling, yoga, elliptical training, and swimming.
- Icing: Apply an ice pack covered in a light towel to painful areas of your foot and/or ankle for up to twenty (20) minutes, three or four times a day.
- Medication: Over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen and naproxen, can reduce pain and inflammation. Check with your healthcare provider before use.
- Immobilization. Sometimes a short-leg cast or boot is worn to immobilize the foot and allow the tendon to heal. You might need to avoid all weight-bearing for a period.
- Physical therapy: Ultrasound therapy and exercises can help rehabilitate the tendon and muscle following immobilization.
How soon after Treatment will I feel better?
Your Posterior Tibial Tendonitis can take several months to heal. You may have to change the ways you approach your daily activities. If Orthotics and braces are not sufficient to reduce your pain and discomfort over a period of six (6) months or more, you may be referred to a foot and ankle surgeon.
When Is Surgical Treatment of Posterior Tibial Tendonitis Needed?
In cases of PTTD that have progressed substantially or have failed to improve with nonsurgical treatment, surgery may be required. The procedure can simply involve removing the inflammatory tissue or replacing an injury. For some advanced cases, surgery may be the only option.
What are the Risks of Surgery?
Every surgery has risks. Risks for this surgery include: excess bleeding, nerve damage, infection, blood clotting, weakness of your calf muscles, and complications from anesthesia Risk of complications vary with age and physical condition.
Diagnosing Posterior Tibial Tendonitis
The telltale sign of Posterior Tibial Tendonitis is localized pain along the inside of your foot and ankle, sometimes stretching up a few inches onto your shin. There is often swelling around the tendon, and the area(s) might be tender or painful to the touch. The best diagnostic test is the single-leg heel raise. People with severe cases of posterior tibial tendon dysfunction can barely get their heel off the ground.
The single-leg heel raise is useful enough that some research articles use it as an inclusion criteria for patients in their studies. The test helps to rule out injuries like medial tibial stress syndrome (shin splints) or a stress fracture of the medial malleolus. With a healthy tendon, you should be able to complete eight to 10 heel raises comfortably. In the early stages of Posterior Tibial Tendonitis, it may not be possible to complete one single heel rise.

Your healthcare provider may move your foot from side to side and check your ankle’s range of motion. Your provider may examine your foot from behind to observe changes in structure or shape. Your heel may point outward, and your inner arch may rest flat on the ground. The front of your foot may also move away from your body to counterbalance the changes to the heel and inner arch. From behind your foot, your provider will also look for a “too many toes” sign. In a normal foot, only the fifth toe (pinky toe) and part or all of the fourth toe (ring toe) are visible on the outside of the foot. In those with PTTD, more toes may be visible.
Doctors may order an MRI scan if exam results are not clear. An MRI can help determine if an area of Tendon has been ruptured, and reveals inflammation around the Tendon(s).
Doctors may use a varieties of diagnostic measures to evaluate your Posterior Tibial Tendonitis, including:
How can I reduce reduce my risk of Posterior Tibial Tendonitis?
You can do a great deal to manage and prevent Posterior Tibial Tendonitis. Here are some very achievable actions that reduce the risk of Posterior Tibial Tendonitis:
- Wear Supportive Footwear. Choose shoes that provides extra arch support. Avoid footwear that can increase your risk of injury, including high heels, platform shoes and flip-flops.
- Stretch Your Lower Legs. Standing calf stretches are a great way to stretch the tendon and the muscles that surround it. A foam roller can also loosen your calf muscles.
- Perform Strengthening Exercises. Resistance band exercises, single-limb heel rises, walking on your toes over a short distance can strengthen your foot and ankle to help prevent injuries.
- Not Pushing Through Pain. When you experience discomfort, stop your activity.
Injuries to the foot or ankle can be frustrating. It is always best to stop any activity that is causing you pain. Rest and over-the-counter or home remedies can treat Posterior Tibial Tendonitis in its earliest stages. In later stages, you may need to see a foot and ankle specialist who will review more detailed treatment options with you.
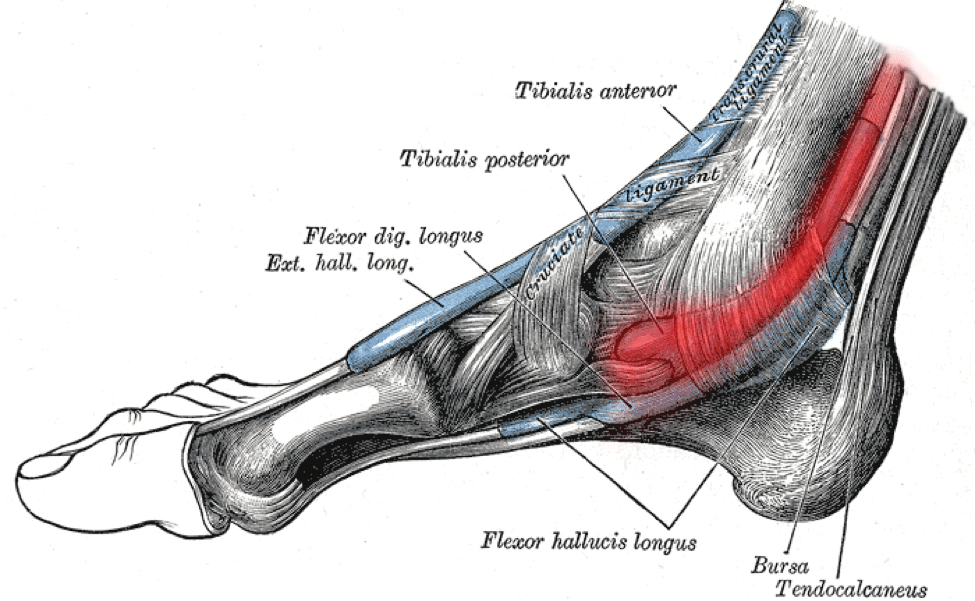
Clinically Relevant Anatomy
The Tibialis Posterior Muscle begins in the back of the lower leg, and its tendon runs around the inside of the ankle and inserts into various areas of the foot. This muscle supports the medial longitudinal arch of the foot, controlling how much and how fast the foot can roll in, or “pronate.”
Tibialis posterior originates from the posterolateral tibia, posteromedial fibula and interosseous membrane.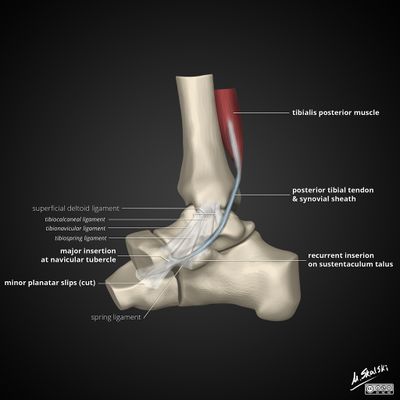
It runs through the deep posterior compartment of the leg and its tendon passes behind the medial malleolus. Tibialis posterior acts as the primary dynamic stabilizer of the medial longitudinal arch and main inverter of the midfoot. Its contraction also elevates the medial longitudinal arch, causing the hindfoot and midfoot to become a rigid structure. This allows the gastrocnemius to act with greater efficiency during the gait cycle[1]
Characteristics / Clinical Presentation
Most patients report a slow, insidious onset of unilateral flatfoot deformity.
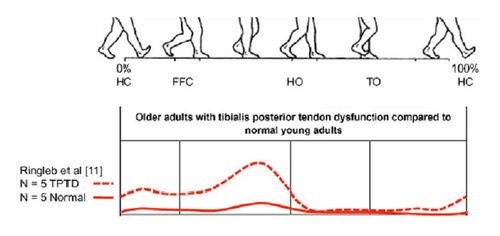
The Posterior Tibial Tendon During Gait
The functions of a healthy tendon are plantar flexion of the ankle, inversion of the foot and elevation of the medial longitudinal arch of the foot. This elevation of the medial longitudinal arch causes a locked entire of the mid-tarsal bones, so the midfoot and hindfoot are stiff.
- This allows the muscle gastrocnemius to act more efficiently during gait.
- With Posterior Tibial Tendonitis the other joint capsules and ligaments become weak. The subtalar joint everts, foot abducts (talonavicular joint) and heel is in valgus position.
- A flattened arch develops what can cause an adult acquired flatfoot.
- Gastrocnemius is unable to act without the posterior tibial tendon what results in affected balance and gait.
Differential Diagnosis
Diagnoses listed below can present very similarly to Posterior Tibial Tendonitis and are often cause for misdiagnosis:
- Tarsal coalition
- Inflammatory arthritis
- Charcot arthropathy
- Neuromuscular disease
- Traumatic disruption of midfoot ligaments[2]
Nonsurgical Treatment
Because of the progressive nature of Posterior Tibial Tendonitis, early treatment is advised. If treated early enough, your symptoms may resolve without the need for surgery, and progression of your condition can be arrested. In contrast, untreated Posterior Tibial Tendonitis could leave you with an extremely flat foot, painful arthritis in the foot and ankle and increasing limitations on walking, running or other activities.
In many cases of Posterior Tibial Tendonitis, the right treatment begins with Orthotics.
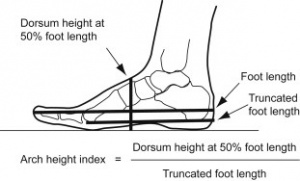
To give your arch the support it needs, your healthcare expert may recommend a custom orthotic device that fits into your shoes to better align your gait. Shoe inserts for posterior tibial tendonitis are used to improve your foot position and raise or support your foot's medial arch, relieving stress and strain on your Tibialis Posterior Tendon.
Orthotic insoles are an extremely cost effective treatment for early stage Posterior Tibial Tendonitis
Orthotics maintain the foot and ankle in a neutral position, and forestall the development of deformity, while decrease the patient's pain and improving function. To achieve this, orthotic insoles are custom-fitted to provide extra cushioning to the arches of feet and the metatarsals. Orthotics play important roles in optimal weight distribution.
"Orthoses can improve foot and ankle alignment, clinical symptoms, and functional outcomes in PTTD patients, with success rates up to 90%."
Posterior Tibial Tendonitis Orthotics play a vital role in the treatment of Posterior Tibial Tendonitis. They help optimize foot loading, supporting and maintaining the arch, and improving the foot biomechanics.
Are Custom Orthotics Worth Money?
"Essentially, yes, custom orthotics are worth it for Posterior Tibial Tendonitis."
"The medical literature supports the use of orthotic devices in patients with posterior tibial tendon dysfunction, especially those in the early stages. Demonstrated benefits include improvements in foot and ankle alignment, clinical symptoms, and functional outcomes". - Holly Olszewski, CPO Orthotic treatments for PTTD aim to decrease the patient’s pain, allow for increased activity and function, maintain a neutral foot and ankle position, and prevent or postpone progression of deformity.8,20,22-38 The literature suggests that orthotic intervention can be successful for a majority of PTTD patients.20,31-3
Correcting Foot Position With Orthotics
Orthotics support the medial arch, and the inner aspect of your foot. There are different types of Orthotics. Off-the-shelf shoe inserts can be purchased at your local shoe store or pharmacy. They are generic orthotics that you place in your shoes to give more support to your feet. These Orthotics are typically low cost, but they are not customized to your exact foot position, and don't offer the same benefits as custom Orthotics
Custom Molded Orthotics are a more effective option
Custom Orthotics are molded to fit your feet by a PT or Orthotist. Often your healthcare provider will take a cast of your feet and then send those casts to an orthotics manufacturer. Many custom shoe inserts can cost $300 to $500 (US). Orthoticsdirect.ca offer excellent Orthotics at a great value.
OrthoticsDirect has simplified this process and enabled people to get custom orthotics without visiting a healthcare provider.
